Public Health Rallies to 'Flatten the Curve'
The public health world and its allies have adopted a rallying cry in the onslaught of the COVID-19 pandemic—"flatten the curve.” As any Columbia Mailman School student will tell you, the concept from infectious disease epidemiology describes the intent of actions to slow the spread of an outbreak.
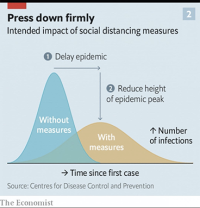
News stories and social media have popularized the notion with a chart showing two divergent curves of the outbreak’s progression—one a steep mountain in which new cases and fatalities happen quickly and in great numbers, the other a gentler hill where the number of new cases is spread out over a longer period of time. One popular version of the chart appeared in The Economist magazine; the chart’s title appeals for measures to “press down firmly.” A lighthearted take transforms the twin curves into feline shapes (its title: “catten the curve”).
“It’s not so much a question of if this [pandemic] will happen anymore but rather more a question of exactly when it will happen and how many people in this country will have severe illness,” said Nancy Messonnier, director of the Center for the National Center for Immunization and Respiratory Diseases at the U.S. Centers for Disease Control and Prevention, at a late February briefing.
As COVID-19 spreads around the world, we’ve seen many actions taken to flatten the curve—some common sense, others bold and unprecedented.
On an individual level, we can all elevate our personal hygiene by regularly and thoroughly washing our hands. We can practice social distancing by forgoing shaking hands (tap elbows instead, if you’d like). And we can ask our employers to allow us to work from home. All these actions protect both ourselves and others.
While some forms of social distancing are done by choice, others have been strictly enforced. In late January, with the COVID-19 cases rising exponentially, China imposed travel restrictions affecting a staggering 780 million people—nearly half of the country’s population. Research by Columbia Mailman School Professors Jeffrey Shaman and Wan Yang found that China’s response helped slow the spread of the outbreak. In other words, it flattened the curve.
More recently, we’ve seen other countries take similar measures to restrict movement. On March 9, Italy announced travel restrictions within its borders; on March 11, the country shuttered all stores except groceries and pharmacies. The same day, President Donald Trump announced plans to restrict air travel from Europe to the United States.
Several U.S. governors, too, have restricted large gatherings. Meanwhile, museums and theaters have shut their doors, and many universities have temporarily switched to remote learning—Columbia included. On the local level, public health authorities are employing epidemiological detective work to track down, test, and isolate people who may have been exposed. (By the time you read this article, many more measures will surely be in place.)
Stephen Morse, a professor of epidemiology and a foremost expert on emerging infectious diseases, explains the rationale for these measures.
“What a lot of countries and localities are doing now is trying to prevent the transmission of this infection by identifying cases and then trying to restrict the further movement of people who might be infected,” he says. “You can slow the rate of transmission so it takes longer for people to come into contact with someone who is infected. In the absence of these measures, you would see the number of infected people rising very quickly. But if you can tamp it down and prevent it, you would slow down the progress of the infection.”
The reason recent measures to flatten the curve of new coronavirus cases have been so bold is that COVID-19 spreads so readily—roughly as contagious as a severe seasonal flu outbreak. Unlike influenza cases, which are spread out over many months, COVID-19 cases can increase very quickly over a matter of weeks. More alarming than the total number of infected people is the total number of acute infections at the same time.
COVID-19 is estimated to be at least 10 times more fatal than the flu, which means flattening the curve is a powerful way to prevent infections and save lives. Hospitals will be better able to care both for patients infected with COVID-19 and those with other urgent health needs.
Measures to slow the outbreak also buy time for scientists to develop better diagnostics, therapies, and eventually a vaccine. Furthermore, if the worst of the pandemic can be delayed until the spring or summer, the healthcare system will be less burdened with influenza patients.
Research shows that the sooner officials encourage people to distance and protect themselves, the more these measures are able to save lives and prevent infections. Once an outbreak gets to the point where cases are spreading within a community, these measures are less effective. In Italy, where the outbreak is severe, hospitals have been overwhelmed with coronavirus cases, a situation that has forced physicians to triage patients.
“The goal is to have fewer people going into the hospital or needing attention at any given time. We want to prevent the big peaks that would put a tremendous burden on healthcare facilities,” says Morse. “Here in the U.S., we’re really not prepared for the kind of case numbers that China had to deal with and the level of medical response they were able to muster.”
While critically important, public health measures to flatten the curve may be impossible to sustain indefinitely. “The question is how long these measures can be sustained before the pandemic breaks out of the cage we are trying to put it in and becomes more like an influenza pandemic,” Morse says. “We still don’t know the answer but I’m afraid we may find out soon enough. In the meantime, we must persist in doing what we can to protect ourselves.”